Clinical Study on Invisible Water Loss of Burn Wounds Treate
作者:Rong Xiang Xu 出版社:KARGER 发行日期:In 2004INTRODUCTION
It has been confirmed that treatment with BRT with MEBT/MEBO offers a unique ability to inhibit excessive loss of water evaporation through the burn wound surface [1-4]. However, there has not been adequate quantitative clinical research at this time. In this study, the authors observed minimal dehydration of burns wounds treated with BRT with MEBT/MEBO in 25 burn patients with different area and different depths compared to the water evaporation value of wound to that of normal skin.
MATERIALS AND METHODS
Twenty-five acute burns patients, 21 males and 4 females, were hospitalized within 6 h after injury. Burn area ranged from 4 % total body surface area (TBSA) to 95 % TBSA. After simple debridement, all patients were treated with BRT with MEBT/MEBO[5]. Observation at 6, 24, 48 and 72 h postburn measured the water evaporation capacity of superficial second-degree, deep second-degree and third-degree wounds, compared to normal skin as a control. In 4 cases with burn area over 50 % TBSA, their daily amounts of water evaporation were determined based on wound evaporation and body surface area. During the liquefaction period, 12 cases with deep second-degree and third-degree wounds received semi-exposed MEBO treatment, and their wound water evaporation was compared with those receiving exposed MEBO treatment.
A Model EPIC evaporometer (Servomed) was used to measure wound water evaporation [6]. Measurement was done at 2 h after application of MEBO, in a room sheltered from the wind. Room temperature was kept at 32C~36C with a relative humidity of 45%~62%.
RESULTS
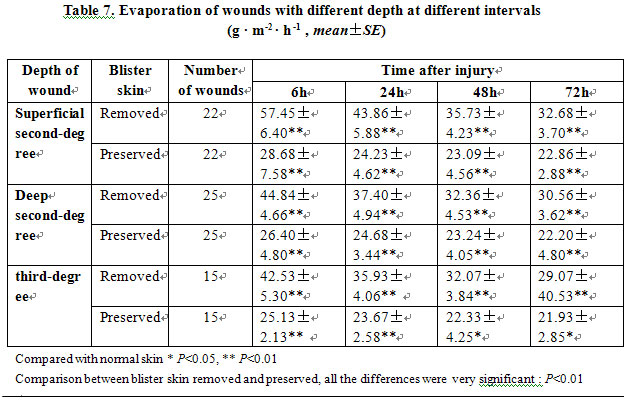
Normal skin water evaporation of the 25 burn patients had an average value of 18.48±5.02 g • m-2 • h -1. Wounds were classified according to their depths and one typical wound from each degree was selected randomly. Blister skin (necrotic epidermis) of every selected typical wound was divided in half with one half remaining intact and the other half having its protective skin removed. Then the evaporation of both halves of the wound was measured, respectively. The results revealed that water evaporation in wounds with preserved epidermis had a very significantly lower evaporation capacity than those with epidermis removed (P<0.01). Water evaporation reached its peak at 6 h postburn and then decreased, but still remained markedly higher than that of the normal skin (P<0.05). For very deep wounds, water evaporation of wounds with epidermis tended to decrease (P<0.05), while evaporation in wounds with preserved epidermis did not decrease significantly (P>0.05, Table 7).
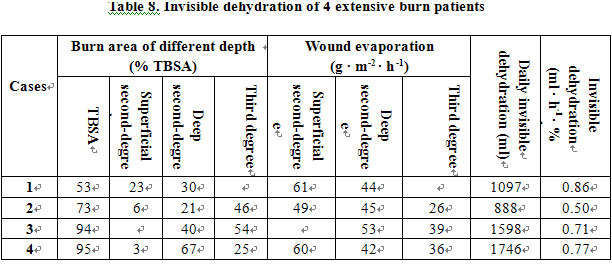
In 4 extensive burns patients with burn area over 50 % TBSA, their total body surface area and burns areas were measured. Daily water evaporations of the wounds with different depths were calculated, respectively. Then invisible dehydration per hour per 1% of second- and third-degree wounds can be obtained. The average value was 0.71 ml • h-1 • % TBSA-1 (Table 8).
During the liquefaction period, deep wounds were treated with exposed or semi-exposed method, the two methods did not result in a significant difference in wound water evaporation (P>0.05, Table 9).

CONCLUSION
(1) BRT with MEBT/MEBO effectively inhibited water evaporation from wounds and decreased total body fluid loss. Additionally, preservation of necrotic epidermis, including blister skin, also helped to decrease water loss.
(2) The fluid injection of burns patients in the early stage postburn follows the formula: 0.4-1.2ml/(h x % BSA), with adjustment according to the depth of the wound and exfoliation of the epidermis.
(3) During the liquefaction period, MEBO could be applied in either the exposed or the semi-exposed mode.
DISCUSSION
Skin is the surface barrier of the human body. As such, it plays an important role in maintaining body fluid status. Burn injury causes damage of this barrier and increases vascular permeability, causing a significant rate of increase of dehydration. Loss of body fluid through burns wounds is proportional to the burn area and depth as well as being related to burn intervals postburn [7]. The results of this study showed that water loss through the wound in the first few days postburn was much greater than through normal skin (P<0.05) and reached its peak at 6 h postburn, then tended to decline and gradually decreased along with the deepening of wound. Preservation of necrotic epidermis, including blistered skin, also helped to decrease water loss. Previous studies gave similar results [8, 9]. However, our degree of local wound water loss was much less than that of those previous reports due to the use of the BRT protocol (MEBT/MEBO) to treat the wounds. We conclude is that BRT reduced wound exudation and inhibited evaporation.
Increased capillary permeability causes exudation of body fluid into the interstitial space, thus forming “burn edema”. Another pathway of water loss is invisible dehydration through the burn wound. In this study with 4 cases having burn area over 50 % TBSA, the average water loss per hour per 1 % of second-degree and third-degree wound water loss was 0.71 ml. It would be helpful to evaluate the volume of fluid resuscitation during the shock stage postburn. Based on this study, the fluid injection of burns patients in the early stage postburn can follow the formula: 0.4-1.2ml/(h x % BSA), also adjust according to the depth of the wound and the exfoliation of the epidermis.
MEBT suggests application of MEBO ointment with the exposed method, but in some cases, the semi-exposed method may be also advisable. The efficacy of the semi-exposed method was comparable to that of the exposed method. Our limited experiment proved that there was no significant difference of the wound water evaporation between the two methods during the liquefaction period (P>0.05), indicating application of MEBO with the exposed or semi-exposed methods had a similar efficacy on inhibiting water loss from the wound surface. It is interesting to note that wound water evaporation measured at the liquefaction period was greater than during the edema resorption period. This might be due to the requirement of more water for the liquefied reaction between MEBO and necrotic tissues as well as the production of liquefaction products.
REFERENCES
1. Xu RX. Moist Exposed Burn Therapy (MEBT): Textbook for Technological Training. Beijing: Beijing Guangming Chinese Medicine Institute for Burns, Wounds and Ulcers, 1989, pp 160-168.
2. Wang CC, Pu ZB, Liu HB, et al: Experimental study on maintaining physiological moist effect of moist exposed burn therapy/moist exposed burn ointment on treating burn wound. Chin J Burns Wounds Surface Ulcers, 1998; 10: 18-20.
3. Zhang LX, Yang KF: Clinical investigation on moist exposed burn therapy:A report of 2076 cases. Chin J Burns Wounds Surface Ulcers, 1989; 1: 22-26.
4. Fu QL, Geng MZ: The early treatment of moderate and severe burns and its theoretical Basis. Chin J Burns Wounds Surface Ulcers, 1992, 4: 1-3.
5. Xu RX: The principle of burn wound management. Proc Natl Conf Burns, Binzhou, 1992.
6. Operating Manual of Model EPIC Servomed Evaporometer. Sweden, 1981.
7. Fang ZY, Wu ZL, Gao XS, Xu FX (eds): The Theory and Practice of Burns. Shenyang, Liaoning Science and Technology Press, 1989, pp 64-274.
8. Davies JWL. The fluid therapy given to 1027 patients during the first 48 h after burning. 1. Total fluid and colloid input. Burns 1975; 1: 319-324.
9. Ge SD, et al. Research on local invisible dehydration of burn wound. Chin J Plast Burn Surg, 1985; 1: 10-12.