Comparative study of the effects of Moist-Exposed Burn Ointm
作者:Rong Xiang Xu 出版社:KARGER 发行日期:In 2004INTRODUCTION
Since 1964 when Teplitz et al. [1] successfully established a representative animal model, burn wound invasive infection has been regarded as one of the main causes of burn-related death. Therefore, topical use of antibacterial agents has played an important role in the control of burn wound infection. In the 1960s, antibacterial agents were developed including sulfamylon [2], silver nitrate [3] and silver sulfadiazine (SD-Ag) [4]. Although SD-Ag has been widely used historically because of its risk/benefit ratio, we now are discouraged by its tendency to enhance drug resistance [5, 6]. Researchers have addressed this weakness in SD-Ag therapy by developing other antimicrobial agents to fight against burn wound infection caused by Pseudomonas aeruginosa and other bacteria. These newer agents include a variety of other topical agents such as silver pipram [7, 8], silver norfloxacin [9, 10] and MEBO [11]. We designed a comparative study to verify the effects of MEBO, SD-Ag and hot dry exposed therapy on controlling P.aeruginosa invasive infection of burns wounds.
MATERIALS AND METHODS
Pathogenic P. aeruginosa was collected from burns wounds of invasive infection, cultured for 16~24 h, then produced into a 4108 suspension using normal saline.
One hundred and twenty healthy adult Wistar rats of either sex weighing 100~200 g were anaesthetized intraperitoneally with sodium pentobarbital (40 mg/kg), shaved of dorsum hair, and scalded on the back with 100°C water for 10 s to each form a full-thickness burn wound with 20 % BSA (determined by pathological examination) [1]. A 1-ml suspension containing 4108 P. aeruginosa was smeared evenly onto the wound surfaces to achieve contamination and infection. The animals were kept in separate cages, and divided randomly into 4 groups as follows (30 in each). Group 1 (control group) received no treatment. Group 2 (MEBO Group) was treated with MEBO according to the method of BRT with MEBT/MEBO which kept the wound moisturized and covered by MEBO throughout the duration of the study. Group 3 (SD-Ag group) was treated with 1 % SD-Ag cold cream, which was applied once a day. Prior to each administration of the SD-Ag, the residual cream and necrotic tissues was wiped off according to the SD-Ag protocol. Group 4 was treated with continuous hot, dry-exposed therapy using a heat-controlled air fan to keep the wound dry.
Six animals in each group were killed under aseptic manipulation at the 1st, 3rd, 5th, 7th, 9th days after treatment. A sample of heart blood was collected and cultured and a specimen of wound skin tissue was taken by sterile scalpel, as deep as the muscular fascia [12] and then cut into two parts. One part was used for bacterial count in sub-eschar viable tissue. The other was fixed in formalin for pathological examination. Sections were observed under a light microscope and the extent of bacterial invasion was classified according to three grades: “0” referring to absence of bacterium; “I” to invasion of bacteria to necrotic tissues; and “II” to invasion of bacteria to viable tissues.
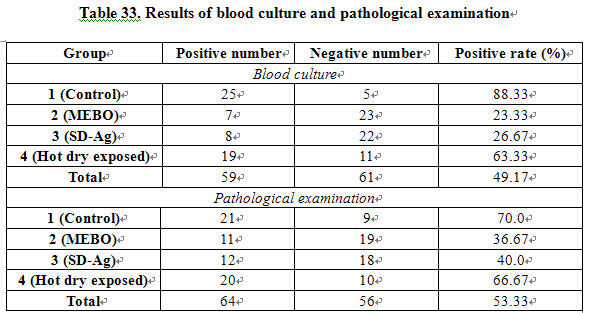
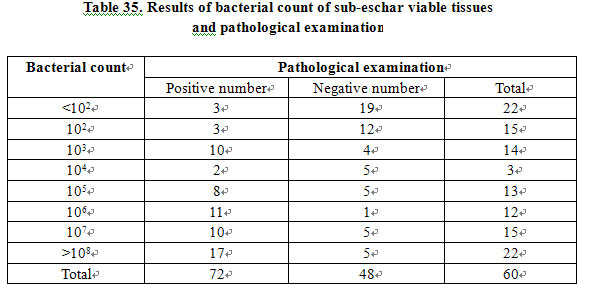
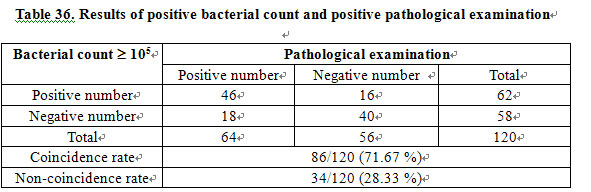
RESULTS CONCLUSION DISCUSSION 1) Evaluation of Antibacterial Effect of Hot Dry-Exposed Therapy: In 1949, Wallace introduced the concept of dry-exposed burns therapy [16,17] in which wound was directly exposed to air at a certain temperature. He believed that direct exposure of the wound might allow the formation of a layer of dry eschar/crust by exudation and necrotic tissue on the wound surface, which served as a barrier against the bacterial contamination. Our study showed that comparing the hot dry-exposed therapy group to untreated control group, there was no obvious difference with respect to bacterial count of sub-eschar viable tissue, positive rate of blood culture and positive rate of pathological examination. We now suggest that the hot, dry-exposed therapy has no significant effect on controlling invasive infection with P. aeruginosa of third-degree burns wounds. 2) Moist exposed burn ointment (MEBO) ---- new topical drug for burns: Infection is the leading cause of death due to burns complications, and burn wound infection is of great clinical concern as it can result in burn wound sepsis and septicemia. An enormous amount of research has been conducted in this field which has produced many advances in burn infection treatment. However, the very existence of necrotic tissue in deep burns provides culture medium conducive to the growth of pathological micro-organisms. Furthermore, the blocked local blood circulation hinders the delivery of anti-bacterial and immune-enhancing peptides which are integral to host-defense competency. Mafenide (Sulfamylon), silver nitrate and SD-Ag were developed in the 1960s [2- 4]. Sulfamylon is a useful antimicrobial agent which penetrates into eschar but has the disadvantage of inhibiting carbonic anhydrase. Therefore, absorption of topical Sulfamylon may result in metabolic acidosis that limits its use in larger burn areas. Silver nitrate was the initial topical agent but its tendency to stain discouraged widespread use. SD-Ag has a strong antimicrobial effect which, despite its poor penetration into eschar, made it the topical agent of choice against burn infection. Our study gave a good proof for this. In order to improve the antimicrobial effect of a topical agent while reducing deleterious side effects, researchers developed other metal sulfonamides such as zinc, ammonium, cerium and erbium for topical therapy [18-21]. However, a comparison of relative antimicrobial effects showed SD-Ag to be the best of the lot,so it remained the agent of choice against P. aeruginosa. This remained the case despite its worrisome profile of creating multidrug resistance[5,6]. Great efforts have been made to deal with P. aeruginosa resistance to SD-Ag. In the 1970s, on the basis of nalidixic acid, great improvements were attained in the research of pyridine, pefloxacin and its derivative in the prevention and treatment of burn infection [7, 8, 22]. Recently, silver norfloxacin has emerged, which was found to be effective in he treatment of P. aeruginosa with drug resistance to SD-Ag [9, 10]. In 1988, a new topical drug for burns wounds was invented, called moist-exposed burn ointment (MEBO) [11]. This innovation has become widely accepted in clinical use [23-26]. In this study, animals with infection of third-degree burns wounds by P. aeruginosa were used, and the comparison showed that MEBO was effective in controlling burn wound P. aeruginosa infection. MEBO had a similar effect to SD-Ag in reducing the bacterial concentration of sub-eschar viable tissues, positive rate of blood culture and incidence of invasion infection. In addition to its ability to kill P. aeruginosa, the other advantages of MEBO are as follows: easy to apply; non-painful, no need for excruciating debridement between applications, and easy assessment of healing progression. It suggested that MEBO was a useful alternative topical drug for burn treatment. Further investigation is needed in order to find whether MEBO controls the infection of other bacteria and micro-organism as well as the mechanism of MEBO against P. aeruginosa. 3) Roles of Bacterial Count of Sub-eschar Viable Tissues and Pathological Examination in the Diagnosis of Burn Wound Infection: Infection has long been one of major life-threatening causes of burn victims. The extent of infection depends on the invasiveness of the pathogenic micro-organism and the power of host resistance [12]. Micro-organism invasiveness has a close correlation to the strains, toxicity and quantity. Therefore, a variety of methods for determining the bacterial count on burns wounds have been developed. As early as 1964, Teplitz et al [1] put forward the concept of burn wound invasive infection. They defined wound invasive infection as occurring when bacterial count exceeded 105 organisms per gram of sub-eschar viable tissue with bacteria penetrating into the underlying tissue and blood vessels. Many researches agree that a bacterial count of 105/g sub-eschar viable tissue was a pivotal level with wounds containing more than 105/g being predisposed to invasive infection [14, 15]. Therefore, the value of 105/g of viable tissue is used as one indicator to predict and diagnose burn wound invasive infection. However, in a comparative study between bacterial count of sub-eschar viable tissue and pathological examination of 200 cases, McManus [26] found that only 35.7 % of tissue specimen with ≥ 105/gram eschar viable tissue demonstrated invasive infection by pathological examination. They concluded that the bacterial density level of 105 or more organisms per gram of sub-eschar viable tissue was not a sufficient indicator for the diagnosis of burn wound invasive. In our study, we made a bacterial count on the sub-eschar viable tissues and performed pathological examination of 120 animals with the results showing a linear correlation between bacterial count and positive rate of pathological examination. The positive rate of pathological examination increased as bacterial density did, and there was a positive relationship (P<0.005). Among 62 specimens showing bacterial count 105/g, 46 were were found positive in pathological examination with a positive rate of 74.2 %. Of 58 specimens showing bacterial count <105/g, 40 were found to be negative in pathological examination with a rate of 69 %. The coincidence rate of both diagnostic methods was 71.67 %. The statistical data demonstrated that if a bacterial count 105/g was used as the critical level in the diagnosis of burn wound invasive infection, there was a significant relationship between the two methods. Therefore, the results of this study suggested that bacterial count on sub-eschar viable tissue remained one of the feasible methods for the prediction and diagnosis of burn wound invasive infection. Although it directly reveals the invasive extent of burn wound invasive infection, pathological examination can give false-negative results due to the impact of many factors including sampling, section and staining techniques. Thus, we must keep in mind that pathological examination for the diagnosis of burn wound invasive infection has its limitations and should not be the sole criteria. Similarily, blood culture has its limitations in that it may result in a low positive rate and delay appearance [27]. Therefore, we conclude that bacterial count of sub-eschar viable tissue can still be used as one of the feasible methods in the early diagnosis of burn wound invasive infection. REFERENCE
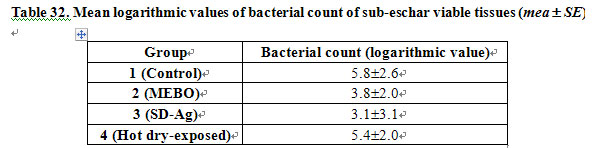
1) Bacterial Count of Sub-Eeschar Viable Tissues: Table 32 shows the mean logarithmic values of bacterial count of sub-eschar viable tissues in each group. The results indicated the mean values in groups 2 and 3 were significantly lower than those in groups 1 and 4 (P<0.01). No marked difference of this value was noted between groups 2 and 3 (P>0.05) or between groups 1 and 4 (P>0.05).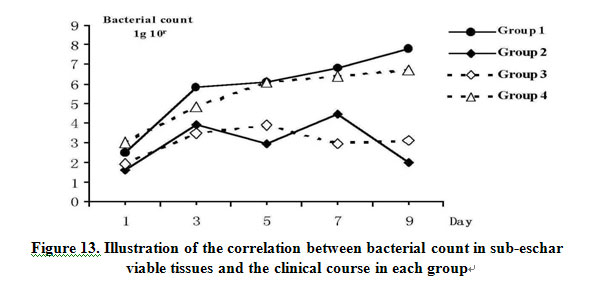
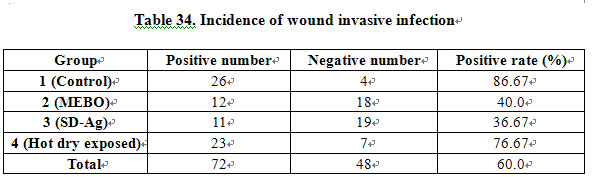
1. MEBO has a similar effect to SD-Ag in controlling burn wound invasive infection by P. aeruginosa.
2. Hot dry-exposed burns therapy has no effect on control third-degree burn wound invasive infection by P. aeruginosa.
3. The bacterial count of sub-eschar viable tissue can still be used as one of the feasible methods in the early diagnosis of burn wound invasive infection.
1. Teplitz C Davis D, et al: Pseudomonas burn wound sepsis. I. Pathogenesis of experimental pseudomonas burn wound sepsis. J Surg Res 1964; 4: 200.
2. Lindberg RB, et al: The successful control of burn wound sepsis. J Trauma 1965; 5: 601.
3. Moyer CA, et al: Treatment of large human burns with 0.5 % silver nitrite solution. Arch Surg 1966; 90: 812.
4. Fox CL Jr. Silver sulfadiazine. Addendum to local therapy of Burns. Rittenburg MS, et al. Med Treat, 1967, 4: 1259.
5. Bridges K, et al. Drug resistance in relation to use of silver sulphadiazine cream in a burn unit. J Clin Pathol, 1977; 30: 160.
6. Heggers JP, et al: The emergence of silver sulphadiazine resistant Pseudomonas aeruginosa. Burns 1978; 5: 184.
7. Ge SD, et al: Experimental study of topical chemotherapy in prevention and treatment of burn infection. Acad J Sec Military Med Coll 1982; 3: 46.
8. Ge SD, et a: Experiment study of topical antimicrobial agent in burns. Chin J Plast Surg Burns 1985; 1: 255.
9. Darrell RW, et al: Norfloxacin and silver norfloxacin in the treatment of pseudomonas corneal ulcer in the rabbit. Trans Am Ophthalmol Soc 1984; 82: 75.
10. Ge SD, et al: The effect of topical use of pyridone antimicrobial agents on preventing and treatment burn infection by Pseudomonas aeruginosa, Chin J Plast Surg Burns 1987; 3: 10.
11. Xu RX: The clinical application of moist exposed burn therapy. Chin J Integr Tradition West Med 1988; 8: 204.
12. Krizek TJ, Robson MC: Evolution of quantitative bacteriology in wound management. Am J Surg 1975; 130: 579.
13. Yang ZJ, Xu WS, Shi JX: Burn management, ed 2. Beijing, People’s Health Press, 1985.
14. Volence FJ, Clark GM, et al: Burn wound biopsy bacterial quantitation: A statistical analysis. Am J Surg 1979; 138: 695.
15. Loebel EC, Marvin JA, et al: The method of quantitative burn wound biopsy cultures and its routine use in the care of the burned patient. Am J Clin Pathol 1974; 61: 20.
16. Wallace AB: Treatment of burn, a return to basic principles. Brit J Plast Surg 1949; 1: 232.
17. Wallace AB: The exposure treatment of burns. Lancet 1951; i : 501.
18. Fox CL Jr., et al: Metal sulfonamides as antibacterial agents in topical therapy. Scand J Plast Reconstr Surg 1977; 13: 89.
19. Monafo WW, et al: Control of infection in major burn wounds by cerium nitrate/silver sulfadiazine. Burns 1977; 3: 104.
20. Fox CL Jr., et al: Topical chemotherapy for burns using cerium salts and silver sulfadiazine. SGO 1977; 104: 668.
21. Ge SD, et al: N 1-metal sulfa drugs and zinepalyanemine and its derivatives in prevention of burn wound sepsis. Chin J Surg 1982; 20: 264.
22. Modak SM, et al: Control of burn wound infection by pefloxacin and derivative. Burns 1984; 10: 170.
23. Zhang LX, Yang KF: Clinical study report: 2076 cases treated with moist exposed burn therapy. Chin J Burns Wounds Ulcers 1989; 1: 22.
24. Zhao RY, Tian LX, Zhao GX: Clinical analysis: 50 cases treated with moist exposed burn therapy. Chin J Burns Wounds Ulcers 1989; 1: 32.
25. Ma EQ, Huang XY, et al: Clinical report of 69 cases treated with moist exposed burn ointment. Chin J Burns Wounds Ulcers 1990; 2: 25.
26. McManus AT, Kim SH: Comparison of quantitative microbiology and histopathology in divided burn wound biopsy specimens. Arch Surg 1987; 122: 74.
27. Baxter CR, Curreri PW, et al: The control of burn wound sepsis by the use of quantitative bacteriologic studies and subeschar clysis with antibiotics. Surg Clin North Am 1973; 53: 1509.